3 challenges to the NHS on its 70th birthday.
NHS embodies a set of key principles and values which are increasingly under attack. In an age of austerity, with widening social and economic inequality, and increasing intergenerational division, I argue that these principles are more relevant and necessary than ever. In this talk for a meeting of the East Dartmoor Labour Party, I look at threats to three of the underpinning principles of the NHS, and considers how we might respond . . .
- NHS celebrates its 70th birthday on 4 July. Timely to look at the challenges it faces, why it is important to be aware of these, and consider how we might respond.
-
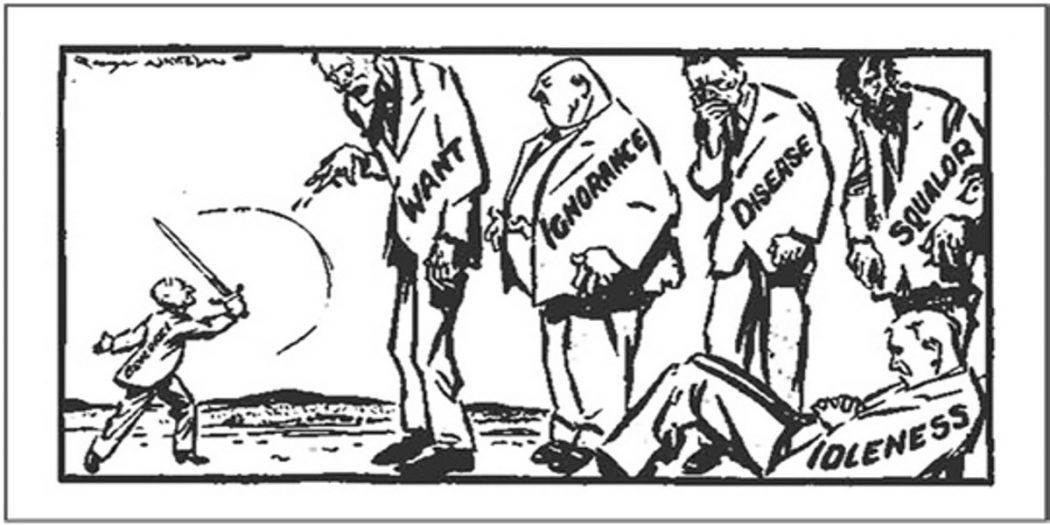
Founded after the WW2 as a key component of Beveridge’s war on the 5 giants (idleness, squalor, want, ignorance, and disease) the HS continues to occupy a unique place in the British psyche. It embodied and continues to embody a set of principles and values: universality, collective citizenship, fairness, social and redistributive justice. It was established as a publicly funded; publicly provided, universal service, free at the point of use.
- NHS was part of a social vision which connects health, housing, education, and employment – we know empirically how health is influenced by each of these – so in that sense challenges to the NHS now are in my view part of a broader neoliberal assault on the entirety of that vision.
-
Throughout the 50s, 60s, and 70s that vision broadly held good. That is not too say that we should be too misty-eyed about these times: financial problems still occurred, waiting lists were too long, and the delivery of services on a universal basis was problematic.
-
It was in the late 80s and 90s that the underpinning principles began to be challenged. The 1990 Act separated for the first-time provision of services from planning (purchasing) and the assessment of need. Under the banner of modernisation later reforms introduced more fully the language and behaviour of the market. The consequences were:
- Entry of new providers into healthcare
- Redefinition of patients as consumers who wanted to express choice
- The business of contracting was invented, a performance management industry (star ratings, performance targets) created
- Regulatory agencies established
- Repetitive, disruptive cycles of organisational change begun (FTs,PCT,CCGs)
- All under the control of New Public Management.
-
This policy direction culminated in the Health and Social Care Act (2012). Directly this absolved the Secretary of State (SoS) of accountability for the NHS, allowed the passage into law of a set of secondary legislation which opened the door for private health insurance schemes, top-up payment schemes, co-payments, and by the introduction of the “any qualified provider” test, heightened the possibility of private sector involvement through the application of competition law to the commissioning of care.
-
HSCA was translated into a vision for the NHS through the Five Year Forward View, which further changed the NHS by creating 44 Sustainability and Transformation Plan geographical footprints for future service design – which in turn are the basis for new care models such as Accountable Care Systems, Accountable Care Organisations, and Integrated Care Organisations.
-
If this is the policy background – let us turn to the key challenges now. My argument is that the current direction of policy is a clear and present danger to the NHS and the principles behind its establishment: and 3 principles in particular: publicly-provided service; universality; publicly-funded.
-
Firstly, public-provision. Consider the growing insertion of private providers within the NHS, and philosophy of marketisation. NHS funding on the private sector has grown from £2.1bn in 2006 to £9bn in 2016. From the early experiments to the most recent examples, a considerable body of evidence has accumulated about private provision which, in summary, shows:
- A market system has created huge transaction costs for the NHS (estimated to cost £4.5bn)
- The inability of regulators to assure patient safety within a profit-motivated private sector (Ian Patterson as the example)
- The significant diversion of funds away from patient care, for example the PFI scheme (Barts Trust pays £127m, pa, until 2049 for its PFI scheme; Central Manchester pays 10% of its annual clinical revenue to the PFI scheme)
- That patients want high quality local services, not artificial choice
- Loss of trust as providers game the targets and avoid accountability
- And that, as with banks in 2008, whilst profit is privatised for shareholders, the risk when providers fail (Carillion) or withdrawn (Circle) is borne entirely by the state.
Despite all this evidence, the national policy response has been to ignore it, and to pursue ever more enthusiastically an irrational, ideologically-driven, zombie policy of privatisation. Thus, we now see new, novel forms of privatisation. In general practice, PUSH Doctor, Doctor at Hand, Babylon and Simply Health are growing
threats to primary care. In community health, Virgin is now a major provider, with over 400 contracts, including here in Devon where it is bidding to extend its control over childrens’ services. And in the acute sector, separate firms are being established to employ hospital staff, whilst land sales are key to hospital financial recovery plans. In summary, the implementation of market reforms has transformed the NHS from a single healthcare system to a complex conglomeration of public and private providers under the umbrella of the NHS brand.
- The second challenge is to the universality of service provision. – the notion that services are broadly the same in Buckfastleigh as in Birmingham. STPs have been explicitly established to solve national problems on a local basis. Direct responsibility has been given to them to make local choices – choices which have primacy over national ones. Looking again at the evidence we see that STPs and CCGs are accentuating local variation through 6 processes, Deflection, Delay, Denial, Selection, Deterrence, and Dilution.
GP referral management schemes delay, defer and deflect patients from secondary care; the explicit exclusion of certain groups (smokers, the obese) denies care; blaming patients for presenting inappropriately deters the future expression of need; the tightening of referral criteria (hip replacements; IVF, continuing care) selects patients, and increasing funding variation in community nursing dilutes quality.
Through these processes geographic variation is being magnified, and the principle of universality undermined. Rather than making transparent the boundaries of care and seeking national agreement on acceptable variation. STPs are developing and implementing their own criteria and policies, the effects of which compound variation and institutionalise the postcode lottery of care.
- The third challenge is funding. At this point speakers generally reveal a graph showing historical NHS expenditure trends, and the debate is framed by international comparisons (relevant or not), anecdotes about efficiency and waste, and discussion about the meaning of the figures and timescales. There is inevitably reference to “infinite” demand.
I’d like to approach it differently. We are constantly told by the rhetoric of austerity that money is tight, that demand is rising (those old people keep living longer and longer), and that difficult choices have to be made.
I want to challenge that. For me, that narrative is about the government trying to locate this funding crisis within the minds of taxpayers and to get them to accept their interpretation of the problem and, also, to be part of the solution by agreeing to new funding alternatives, such as top-up payments, co-payments, by accepting restrictions on access to care for immigrants, or the obese, or by agreeing to use more private healthcare. Moreover, the funding crisis in the NHS is constructed as a purely financial one, predicated upon convincing people that the austere response is the only possible one. Underpinned by notions of staff ineffectiveness and inefficiency, this creates a narrative strong enough to compromise the principle of treatment being free at the point of use.
An alternative narrative is that we are (according to Liam Fox no less) the 5 th largest economy in the world: that 78% of people consistently rate health spending as a priority, and 67% would pay more tax for the NHS. Current health spending has increased (4.1% of GDP in 1978 to 7.2% in 2016; but going down to 6.8% in 2019) but even the promises made by Tony Blair to equal European average spending, have been, in this context, modest. Am I alone in thinking we can and should do better?
The challenge is to resist the dominant narrative that it is a service that can’t be afforded, that the only solutions lie in private care and insurance; that demand rises inexorably, or that a cross-party Royal Commission, or a hypothecated tax, is needed to sort this all out. It can be afforded – it is a question of political will.
- I’ve identified 3 challenges to the principles of the NHS: to universality; to its public provision; and to its national funding. It is often questioned whether the principles, established in 1948, of social justice, collective citizenship, and an active, assertive role for the state are still relevant today. For me, in an age of austerity, with widening economic and social inequality, and increasing inter-generational division, these principles seem more relevant and necessary than ever.
-
How can we respond individually and collectively to the challenges?
A) NHS Reinstatement Bill is being debated in Parliament on 11 July, sponsored by Eleanor Smith. The Bill re-establishes statutory health bodies with responsibility for health and underlines accountability to local people. It reinstates the national accountability of the SoS. Further, it abolishes marketisation, commercial contracting, and
centralises PFI debts. This bill should be widely supported.
B) Local action is key to disseminating the message about what is happening within our health service. There are active campaign groups across the country including the Keep our NHS Public and the NHS 999 campaigns, and local NHS SOS campaigns here in Devon.
C) Real stories, patient experience stories are valuable material on the doorstep when campaigning about the NHS. Its is important to challenge the myth that “there is no money for the NHS,” or that it cannot be afforded, and real examples of the damage that has been done to the NHS, by talking about patient care stories can help
here.
D) Finally, those who understand best the changes that have occurred with the NHS are often those who work within it. Talking to local practice and community staff, going to see hospital staff, is an effective way of learning about what is happening, and building allies and future supporters.
