Promoting patient choice at the end of life
Labour’s health and care policy recognises that “users, their families and the public are at the heart of local health and care services”. To that end the policy stresses the importance of respecting a person’s choice of care setting at the end of life, with the ambition of making it possible for people to die at home surrounded by their family.
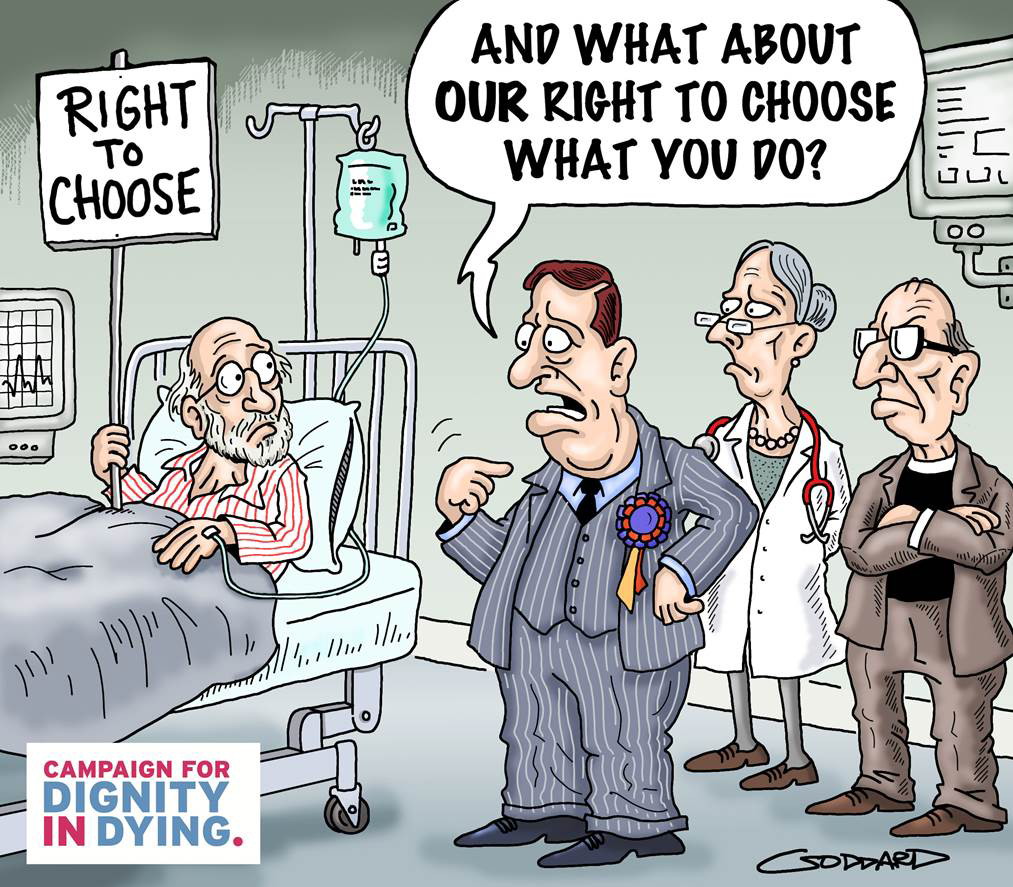
This is a welcome commitment; but it is important to recognise that personal control at the end of life extends beyond choice of care setting and includes choice and control over how and when we die.
Historically policy on end-of-life care and decision making has developed in a piecemeal way. This is partly because of the ethical dimension. On some issues Government can set out policy (like dying at home) but others are issues of conscience and are for Parliament to decide (like assisted dying for the terminally ill). At times Government can get caught between the two (like the right to refuse life-sustaining treatment and the debate around the Liverpool Care Pathway).
A failure to look holistically at patient choice at the end of life means that some significant issues remain unresolved. End-of-life care has been included as a priority in the most recent NHS Mandate, but NHS England has stated that it will not be refreshing the End of Life Care Strategy, instead publishing a set of actions and ambitions – leading the National Council for Palliative Care to express concerns that momentum will be lost in delivering improved access to end-of-life care. On the ground the Liverpool Care Pathway, following an independent review, is being phased out, but with no firm replacement in terms of national guidelines for healthcare professionals. Concerns have also been raised about the lack of a national policy on do not attempt resuscitation (DNAR) orders, and more widely a failure to promote patients’ existing rights through Advance Decisions and Lasting Powers of Attorney to refuse medical treatment in advance of a loss of capacity. And of course there is the ongoing public and parliamentary debate on assisted dying for the terminally ill, with a Private Members’ Bill tabled by Lord Falconer set to be debated shortly in the House of Lords.
Medical advances mean that thankfully many of us will now live longer, but also that many more of us will face prolonged suffering at the end of life. Patients who now rightly expect their wishes and autonomy to be respected in all other areas of healthcare will no longer accept limited choice at the end of life and/or having to watch loved ones suffer against their wishes. Acknowledging the ethical dimension in end-of-life care, there is a real need for leadership from a future Labour Government in creating the framework and making parliamentary time available to consider these issues in the round.
In short, the Labour Manifesto should provide a broader commitment to promoting patient choice at the end of life. Specifically, we hope that a future Labour Government would, in addition to promoting choice over care setting at the end of life, ensure:
Access to good quality end-of-life care across all care settings including hospitals and care homes.
- Sufficient training in end-of-life care for relevant healthcare professionals, including good communication with patients, and clear guidance on removing or withholding life-sustaining treatment.
- Promotion of advance care planning, and the ability for patients to set out through Advance Decisions and Lasting Powers of Attorney their treatment wishes in advance of a loss of capacity.
- Sufficient parliamentary time to debate the issue of assisted dying for terminally ill people.